Fighting for better healthcare with UOPX alumna Roselyn Tso
Listen to the podcast episode featuring UOPX alumna Roselyn Tso
Improving healthcare for Native Americans
Ų▀╔½╩ėŲĄ alumna Roselyn Tso is the retired director of the (IHS), the federal health program for American Indians and Alaska Natives. In this episode of the Degrees of SuccessŌäó podcast, host Freda Richards explores the urgent need for change in the healthcare system serving these populations, from underfunding to other barriers.
0:00
- Tell me about your passion for healthcare
0:02
and what steps you have completed.
0:05
- I've gone to places as the IHS director
0:08
that no other IHS director has visited,
0:12
and that set the stage for, i, I would say, one
0:15
of the most transformative approaches from the federal
0:19
government's perspective, that we can work side by side
0:24
with each of the 574 federally recognized tribes
0:28
in their space
0:30
for their travel communities the way they want it.
0:46
- Hello and welcome to the Degrees of Success podcast.
0:49
I'm your host, Frida Richards,
0:51
and today we have the great honor of having Ms.
0:54
Roselyn Tso join us.
0:56
She is the director of Indian Health Services.
1:00
She's also a member of the Navajo Nation.
1:03
She has a great passion for enhancing healthcare
1:06
for all native Americans.
1:09
And of course, she's a Ų▀╔½╩ėŲĄ alum.
1:12
Help me welcome Ms. Roselyn Tso.
1:14
Tell me how you grew up,
Growing Up in Arizona
1:16
what your childhood was like, and where you're from. So
1:18
- I am from a little town in Arizona.
1:21
It's called Page Arizona, north northern part
1:24
of the state of Arizona.
1:26
I grew up there. I grew up on the Navajo Reservation.
1:29
I'm, I am the daughter of a Korean War veteran.
1:33
I am also the daughter of a
1:36
longtime minister on the Navajo reservation.
1:40
And then my father was a rancher
1:41
and he was also a businessman.
1:43
And my mother's role, she was there side by side with him
1:47
for more than 66 years.
1:48
And so I grew up in a home with imagine a rancher
1:53
and a military and businessman.
1:55
You know, you bring up, you, you, you're raised with a lot
1:57
of structure and a lot of discipline.
2:00
So I, I carry that, those with me.
2:02
I cherish those memories
2:05
and the work that my parents did to raise,
2:07
to raise me as they did.
2:10
And then from there, of course, going to high school
2:13
and in small town,
2:14
and then from there just, just keep moving forward.
2:17
- So what was it like growing up in a small
2:20
town in page Arizona?
2:22
- It was great, you know, I mean, it was great.
2:24
But, you know, the, some of the challenges that I still
2:27
worked through today as, as my job
2:29
as the Indian Health Service, for example, the home
2:32
that I grew up in, we didn't have electricity
2:34
and we didn't have water.
2:35
The home that, that is still there today,
2:37
that was our family home, finally got electricity in 2014,
2:42
and then still today, there's no running water.
2:45
So there are still many, many homes on our tribal,
2:48
tribal lands that don't have sufficient sewer and water
2:52
or even electricity.
2:54
So as, as we talk about healthcare
2:57
and as we talk about public health, those are still factors
Public Health Challenges
3:00
that, that are fundamental needs
3:03
for our people across Indian country.
3:06
- So you have a great passion for your people, as you said,
3:10
your culture wanting to give back,
3:13
growing up in page Arizona, in a home
3:17
that had no electricity,
3:18
or excuse me, no running water, you've been able
3:21
to experience what you're trying to change.
3:26
Tell me clearly that passion comes from your, your childhood
3:30
and experiencing it, but what,
3:31
what else drives you in getting involved in healthcare
3:34
and making a change in the community?
3:36
- Thank you. So there are many, many parts of that
3:39
that great question.
3:41
First is just the challenges
3:43
that our people still live with today.
3:46
I mentioned earlier diabetes, you know, we,
3:49
we have the highest rates of diabetes across any country.
3:54
We have challenges with regards to just
3:57
public health infrastructure that impact our ability
4:01
to raise, you know, raise up some of our travel communities
4:04
to the level that we would like to see them.
4:07
But part part of that was, again, reinforced just recently
4:11
with the Covid pandemic.
4:13
It just reminds me of how important it's that we continue
4:17
to improve our travel communities with that infrastructure,
4:21
that infrastructure builds success,
4:23
that infrastructure build what we need
4:26
for our travel communities
4:27
to be successful as we move forward.
4:30
So whether it is broadband, whether it is improved roads,
4:34
whether it's housing, whether it's food insecurities
4:38
that many of our travel communities live with, all of that
4:42
is impacts a person's health.
4:45
So when we talk about transportation and, and,
4:49
and if we can't get a person from point A to point B
4:52
to their, to their appointments or whatever,
4:54
and not take into consideration transportation, then,
4:58
then we are not addressing the the person's need.
Reconnecting with Traditional Practices
5:01
If we're talking about food insecurities, where many
5:04
of our families today struggle with that across,
5:07
across the nation struggle with food insecurity
5:10
and what do we do about that?
5:11
How do we build sustainability?
5:14
How do we build systems back into our travel communities
5:17
where we're less reliant
5:18
and we go back to some of our traditional practices.
5:21
And so we're seeing this as we move forward.
5:24
We're seeing that progress across Indian country is being
5:29
the most successful places that we see progress.
5:32
It's where travel communities are thriving.
5:35
When they go back to the traditional practices, they go back
5:38
to the traditional foods, they go back
5:40
to the traditional traditions of just, just the, the,
5:45
the practices of customs for dancing and singing
5:49
and those kinds of things
5:50
that are being brought back into their health,
5:52
into their communities.
5:54
There's that, those are the communities
5:56
that are thriving the most.
5:58
And I think that investment that reinvestment
6:00
to tribal communities are, is so important.
6:04
The the flip side of that is also
6:07
that Indian policies of the history, the history
6:11
of Indian policies
6:13
and how they still impact negatively impact tribal
6:17
communities today.
6:19
If you go to just the basic elements
6:22
of Indian policies that were established years
6:26
and years ago, they were to eradicate us.
6:29
They were to do away with the American Indians
6:32
and Alaska native people.
6:33
But as I've traveled throughout,
6:35
particularly over the last 27 months
6:37
to see travel communities thriving,
6:40
to see travel communities say we wanna change the outcomes
6:44
of our, our community so we can be healthier community.
6:47
That has been the best. That has been just an absolute
6:49
rewarding experience.
6:51
And there are other places where,
6:52
and other areas that we still have to work on.
6:56
But I think that we are on the right path to take to,
6:59
to make sure that any country is healthy.
Historical Context and Systemic Issues
7:03
- Well, I'm gonna have to agree, you've been at the helm of
7:06
that will for 27 months.
7:07
So I'm confident as we move forward into this conversation
7:10
and hear more about your accomplishments
7:13
with those native tribes, that we will see that.
7:18
But before that, I, I wanna ask this.
7:21
Tell us the why, why
7:25
were Native American
7:29
or the tribal communities placed in this situation?
7:31
Tell me why this is that it, that it's common for them not
7:35
to have running water or for them to have diabetes.
7:39
Tell me the root, the why.
7:42
- So that, that's a very loaded question
7:46
and I don't feel that I can speak for tribes
7:49
or tribal leaders in, in this particular area.
7:53
But we do know that the lands that, that were, that
7:57
that tribal communities were moved from was part of it.
8:02
And what is on that land?
8:04
What is on that land that those precious minerals
8:07
or whatever, that there was, that the government was looking
8:10
for, to relocate American Indian people from their tribal
8:14
lands to different location.
8:17
That's one of them.
8:18
And and so as we look at the why of where, of why we are
8:23
where we are today, you know, you, you look at just
8:26
the boarding school era where many, many,
8:29
many children were relocated, taken from their families
8:33
and placed in, in government led boarding schools.
8:37
There's just, we've just completed through the,
8:40
the Secretary of Interior just completed a, a study on this
8:45
and the impacts.
8:46
And even though that some of those might have ended in the,
8:50
in the mid sixties, they're still impacting
8:55
the relocation of people taken from their tribal lands
8:59
and relocated into other places that were foreign to them.
9:03
Maybe they could grow things in the land that they used
9:06
to live on, and the new land maybe doesn't support that.
9:10
Maybe there's not that infrastructure, infrastructure
9:13
that's in place for that.
9:14
All of these things, you see, those, those
9:18
to me lead up to the why.
9:20
And so when you look at diabetes,
9:22
when you look at these other challenges that we have
9:25
of heart disease, you know, I,
9:26
we've been working very hard at Indian Health Service
9:30
about food is medicine
9:32
and everything that we take in
9:35
impacts our body one way or another.
9:37
And so if they are unhealthy, if they are not good,
9:42
or if that's not what we were traditionally accustomed
9:45
to eating, then those make a change.
9:48
Moreover, just the environments that we live in,
9:51
I've traveled several times to the state of Alaska
9:54
and just, you know, again, to understand
9:56
and appreciate their challenges just for transportation,
Alaska Visit: Cost and Access Issues
10:00
they have to go, I, I might be able to fly into Anchorage,
10:05
Alaska, but from there to get to any village, this has to be
10:09
by air or by boat.
10:10
There's no roads in Alaska.
10:13
So how do you, how do you, we manage that,
10:15
not just from a healthcare perspective,
10:18
but just the way people live.
10:21
In, in a recent visit that I had, I visited a small village,
10:24
about 500 people,
10:26
and I always like to look in the stores
10:29
of the, the little stores.
10:30
I like to look at how, how their homes
10:32
are and how people live.
10:34
I went into the store
10:35
and it's $14 for a gallon of water,
10:40
14 for a gallon of water,
10:43
and then right next to it, it's maybe a dollar 20
10:47
for a can of soda.
10:49
So you look at those options that people have and,
10:54
and the resources or limited resources that they might have
10:57
if they're choosing the soda because they can afford that.
11:02
The challenge that that creates is
11:04
by the time children are school age,
11:07
they need reconstructive dental work.
11:10
So all of these things that we talk about,
11:13
and that's why I think from a healthcare perspective,
11:16
we have to take a step back
11:18
and really look at those social drivers of health
11:23
and how those impact the health of our community
11:27
because you can't just deal with the, the medical side.
11:31
You can't just deal with the pharmaceutical side
11:33
and say that we've done our part without looking at
11:37
what are these other factors that impact that patient
11:41
and for them to be successful, for them to be
11:44
where we want them to be as healthy tribal communities.
11:48
So it's more than just medical at ihs.
11:52
And when you look at our mission statement,
11:54
we talk about the, the physical, the mental,
11:58
the social and spiritual health of our people.
Holistic Health at IHS
12:02
When you look at it, that that's the whole person.
12:05
And so that does take time as we start
12:08
to really think about, you know, you can,
12:10
you can imagine a if there's not sufficient housing in a
12:13
tribal community, what happens?
12:16
Somebody's worried about that
12:17
and somebody's gonna be impacted by that
12:20
and probably less in thinking of their health.
12:24
So that goes to the bottom of the list until it,
12:28
until it came be at the bottom of the list anymore.
12:31
And then of course, that has its own challenges with it.
12:34
So we know that policies across even policies today continue
12:39
to negatively impact our people.
12:41
But the, at the same time, we have many,
12:45
many travel communities that continue to thrive
12:47
because they are taking the approach
12:50
of addressing the whole person and
12:53
therefore building up each tribal community to be healthier.
12:58
- I heard you say that it's very important for,
13:02
or that you have, there's current, there's current tribes
13:04
that are thriving now that they're having the opportunity
13:08
to invest back into their traditions,
13:11
invest back into the food that that was traditionally
13:15
what they ate prior to being introduced to
13:20
others, other food such as soda
13:23
or maybe burgers or something along those lines.
13:25
I wouldn't necessarily be in line with the native
13:31
nutrition that was done in the past
13:33
or that was participated in the past.
13:36
My question to you is, what,
13:40
what are, what are those foods one that you think that
13:44
are helping the Native Americans get back
13:47
to their health and those traditions?
13:49
And then secondly, I wanted to acknowledge
13:52
that I absolutely agree with you
13:55
and I've seen studies,
13:57
I'm currently getting my doctorate right now
13:59
here at Ų▀╔½╩ėŲĄ.
14:01
And in in those studies I've actually seen that all
14:06
of our bodies are aligned
14:09
to traditional foods.
14:11
Like, so we're not all supposed to be eating the same thing.
14:14
A burger for me is very different.
14:16
Well, my body will handle that very differently than a
14:18
burger for our producer or so on and so forth.
14:21
And so I think that that in itself is very important.
14:25
You're speaking about preventative, eat, eat this food
14:30
to, to prevent having to heal yourself
14:35
or have a medicine save you.
14:39
Tell me more about the food that
14:41
the Native Americans are accustomed to
14:44
that's actually aligning
14:45
with them staying healthy in those traditions.
14:49
- Well, there again, you know, there's over,
14:51
there's over 500,
14:53
actually 574 federally recognized tribes across,
14:58
across the country at the Indian Health Service being the
Region-Based Traditional Foods
15:02
18th largest healthcare system.
15:04
We span about 37 states of where we have those tribes that,
15:08
that live in those 37 states.
15:10
And so, you know, again, taking one
15:13
of those 574 federally recognized tribes and,
15:17
and not layering that we're all like this
15:19
or we're all the same because we're not so
15:22
by regions perhaps.
15:23
So we're different foods that people were, were,
15:25
we're more accustomed to than other regions in Alaska,
15:30
for example, you know, they, they rely on the salmon.
15:34
They, they, that was their choice, that was their food.
15:38
And down in, in the lower 48, they were different kinds
15:41
of foods that that, that were traditionally,
15:45
that our people were traditional accustomed to.
15:47
And those, again, back, back when they were grown
15:52
and then they were utilized.
15:53
And then, so as you, as we,
15:56
so I can't quite answer your question specifically.
15:58
I can talk about maybe this tribe or that tribe,
16:01
but what, what's important to understand is that what I,
16:05
what I experienced as a young child
16:08
and what my parents tried to, what my mother tried
16:11
to prepare for us as, as a young child,
16:13
IWI wouldn't even say we're, we're our traditional foods.
16:17
She was just trying to put food on a table
16:19
that she could put together to, to make sure
16:21
that all all of us ate.
16:23
Children were able to have something to eat
16:26
at any given time.
16:27
So, so I think, I think it's bigger than that.
16:31
And what I see though,
16:33
what I've seen in tribal communities is that each tribe is,
16:37
is making those decisions for themselves.
16:40
What can they, what can they go back to?
16:43
How do they foster that?
16:45
I've been in, in a visiting a tribe in Oklahoma,
16:48
for example, and they have their own little grocery store
16:53
and they put in there what they believe is best
16:57
for their tribal communities they put in there.
17:00
So, so we don't, they don't just go to any grocery store.
17:03
So they're supporting that travel community
17:06
with the healthy choices from, from a a,
17:10
a community perspective.
17:12
And I think that if each community could do that, as opposed
17:15
to what I explained in what I experienced at Alaska
17:18
and what I observed in terms of prices
17:21
and so forth, if those things could be met in each tribal
17:24
community, that's what's gonna drive
17:27
improvement for that community.
17:29
Moreover, coupling that with education today, why it's
17:33
so important that we need to move around, why it's
17:37
so important for us to exercise or walk or whatever it is.
17:41
And many of the services that we do at IHS
17:44
through our diabetes program supports
17:47
that many tribes have taken those resources
17:50
and built wellness centers
17:52
or working on building wellness centers.
17:54
And again, a place, a safe place where people can go
17:57
to do their exercise or to do their walk walking
Role of Education and Wellness Centers
18:01
or just to do food lessons.
18:04
How do you, how do you cook with the foods
18:07
that we have today and how do you make them healthier?
18:10
How do you make these, these quick meals?
18:12
Because we're all busy and we're all running from,
18:15
from point A to point B.
18:16
So I see that happening in tribal communities,
18:19
and if they, each tribal community can really invest in that
18:23
for their people, it's gonna make change.
18:26
It's making changes in our, in our tribal communities.
18:30
- That is very powerful.
18:31
And I wanna hear more about your passion for healthcare
18:36
because again, in my studies I've also found
18:39
that there's like in low income African American communities
18:44
there, there's food scarcity, there's less grocery stores,
18:49
but there'll be in like within five to 10 miles,
18:52
there'll be eight McDonald's, 10 Burger Kings, Wendy's,
18:57
pizza Hut, smoke shops,
19:01
the cash advance stores, all of that within a small amount
19:05
of space and maybe two grocery stores.
19:10
That in itself is completely
19:14
destructive for that community.
19:17
And it is only encouraging them to
19:22
spend money recklessly
19:24
and to possibly indulge in
19:29
tobacco or other things from the smoke shop.
19:31
And then the same thing with the food.
19:33
How much cheaper is it to get a Happy meal
19:35
or something along those lines as opposed to going
19:38
to your grocery store where there's only two of them.
19:42
And to your point, soda is substantially cheaper than the
19:45
healthier options.
19:48
You have made some very important moves
19:51
and changes for your community.
19:53
Tell me about your passion for healthcare
19:56
and what steps you have started within this 27 months
27 Months of Leadership
20:02
and, and completed to help move that forward.
20:08
- Thank you. So Indian Health Service is part
20:10
of the Department of Health and Human Services.
20:13
And through many treaty agreements, through many commitments
20:17
of the federal government, the the exchange for land
20:22
or exchange for resources in Indian country was dependent on
20:27
the government providing healthcare
20:29
to American Indians and Alaska natives.
20:31
That's what makes our relationships
20:33
with the federal government, each tribal relationship
20:36
with the federal government unique
20:38
because it is a nation to nation agreements
20:41
that were had way back when.
20:43
And, and many of those agreements, if not all,
20:46
include a component.
20:48
So Indian Health Service is that federal component.
20:51
We are the, the lead organization, if you will,
20:54
the lead government organization that provides
20:57
that healthcare for American Indians and Alaska natives.
21:01
One of the great things about the Indian Self-Determination
21:05
Act that was developed in 1975 provides
21:10
for tribal governments to assume they're part
21:14
of their healthcare system.
21:16
So since that time, tribes have contracted
21:21
or compacted their part of what I, what the government used
21:25
to pro provide for their tribal communities
21:27
in terms of healthcare.
21:29
Again, that self-determination, that self-governance act
21:34
that tribes have taken now has led IHS
21:38
to be about 40.
21:40
Less than 40% of IHS remains as a federal government.
21:45
The rest, or 60 plus percent
21:48
of the tribes have taken their portion
21:51
of the federal government to provide healthcare for them,
21:54
for their own communities.
21:56
That is thriving.
21:58
That is where the change is going to come,
22:01
is when tribal communities take responsibility
22:04
for their own healthcare
22:06
because they know what is best for their tribal communities.
22:09
The government can't say, oh, we should do this here
22:12
for this tribe, or we think that this is gonna work for no,
22:15
because we're not in their space.
22:17
We're not in those tribal communities.
22:20
We don't know how many grocery stores they
22:23
have or don't have.
22:25
We don't know what resources
22:26
that they have or they don't have.
22:28
So I think as we, as the government keeps moving forward
22:32
and fostering this relationship with the,
22:34
with tribal communities
22:36
and tribal governments, that the more
22:39
that tribal communities can take responsibility
22:42
for their healthcare system
22:44
or for their whole community, that that is
22:48
where they're going to make the best decisions.
22:51
And I think as we continue to embrace
22:53
that from the federal government, our role is to assist.
22:56
Our role is to support our role is to foster those steps
Rural Health Access and Challenges
23:00
that the tribes choose to take.
23:02
I will say, you know, just the amazing work
23:06
that is happening in Indian country as a result
23:08
of self-governance and self-determination on,
23:11
on in Cherokee Nation.
23:13
For example, in Oklahoma,
23:15
we have the first medical school on tribal land.
23:19
So I wish we could have a medical school in every, you know,
23:23
in every region on tribal land.
23:26
But that's the beginning.
23:27
That's the beginning Out in Arizona, we have one
23:30
of the first cancer centers in a tribal community,
23:33
so people don't have to drive hours
23:36
and hours to get to for cancer care.
23:38
So we're getting there.
23:40
They are small steps and we have a long ways to go.
23:43
But the more that tribal governments can take responsibility
23:47
or when they choose to
23:49
and when they want to,
23:50
then they're going to be the catalyst.
23:52
They are making those changes.
23:54
They are showing that we can do this work as we move along.
23:59
And then most of our care is in rural America.
24:02
Most of our care is in, in, in isolated locations
24:06
where we have to drive four hours.
24:10
When you drive from Fort Peck, Montana to get to Billings,
24:14
Montana, if you need higher level of care,
24:16
it's a four hour drive.
24:18
So you're thinking about somebody that has dialysis,
24:21
you're thinking about somebody that's a cancer patient
24:24
and have to make that drive, you know, maybe two
24:27
or three times a week for dialysis.
24:29
How do we change this?
24:31
How do we really look at creative ways
24:34
that we bring services closer to the people in their,
24:37
in their tropical communities And not just for American,
24:39
Amy Alaska names, names for all, for all Americans,
24:43
that we deserve better healthcare across the nation.
24:46
The other thing I would say is that
24:49
over the years we sometimes at Indian Health Service,
24:53
we have made our system more complicated.
24:56
It's navigating the healthcare system today is already
24:59
complicated and we don't need to put more layers on that
25:04
for our American Indians and Alaska native people.
25:07
So dialing it back, simplifying it, going back
25:10
and saying, where do we need to streamline?
25:12
Where do we need to cut out these layers of, of steps
25:17
that maybe our people have to take?
25:19
Those are really important for us to do.
25:21
So as I look at healthcare
25:23
or as I've looked at it while being in this role,
25:26
has really been trying to look at it from that,
25:29
that patient perspective.
25:32
During the last part of my father's life, this is
25:36
my father's a decorated veteran,
25:39
but he chose not to go to the va.
25:42
He chose to go to his,
25:45
his small healthcare facility on the Navajo reservation.
25:49
That was his choice.
25:51
And even though I, I thought you, you have
25:54
the VA owes you this, you, you're entitled to this,
25:57
they're entitled to the best care possible, whether it's IHS
Personal Inspiration and Future Goals
26:02
or the VA or however they choose to do it.
26:05
So, and then I had then I also went
26:07
through the same experience of navigating my mother's care
26:10
as, as a cancer patient.
26:12
She had breast cancer and, and navigating that for her.
26:15
But as, as what I saw with her was that was
26:19
during the pandemic
26:20
and that opened the door for,
26:22
even though it was always there for telehealth or,
26:26
or audio health.
26:28
And so she didn't have to drive as far we could take a call
26:31
with her at home and she didn't have to wait in a car
26:35
or drive in a car for hours to get to her appointment.
26:38
So those things are changing
26:40
as we see technology changing us
26:43
as we see these opportunities to make sure
26:46
that we have better outcomes
26:49
or even better experiences
26:50
for our patients is very, very important.
26:53
That's what drives me.
26:55
That's what reminds me that I see that.
26:58
And then I turn and look at my 5-year-old granddaughter
27:02
and I'm thinking, what do I leave for her?
27:04
What do I, what do I want?
27:06
What do I wanna make sure that my children have care,
27:10
the best care that they should be, that they should have.
27:14
And so they're healthy.
27:15
Not just healthy today,
27:17
but healthy 20 years from now, 40 years from now,
27:20
and 50 years from now.
27:21
So I think all of these things
27:23
that we're talking about when we're talking about these
27:25
social drivers of health, what are we eating?
27:28
How, what am my exam?
27:29
What, what is my responsibility to be an example to her
27:33
and to my grandchildren about what I eat?
27:36
Because we give them what we're eating
27:39
and we're, we're, if, if it's healthy, that's great.
27:42
If it's not, then it's not good.
27:44
'cause then we're just fostering this, these behaviors
27:47
as we continue to drive.
27:48
So that's what drives me every single day.
27:51
The work that I do.
27:52
There's a face at the end of every patient experience.
27:57
When I'm looking at policy, when I'm looking at what is it
28:00
that we're gonna work on at IHS, there's a,
28:03
there's a face there, there, there's an, it's meaningful,
28:06
there's a tribe there,
28:07
there's a tribal leader's voice I can hear saying,
28:11
we want this and we want that,
28:13
and this is the way we want it.
28:15
So again, it's not so much that we, we provide the care
28:18
that way, but we provide the care the way
28:21
in this case, our people want it. Tell
28:24
- Me what's up - Next.
Closing Thoughts and Appreciation
28:25
Well, I'll take a little bit of time for myself.
28:27
I think there, you know, anyone that has been in these kinds
28:30
of positions, you need time to sort of just step away and,
28:35
and, and decompress, if you will, just the,
28:40
the past that, that we have dealt with.
28:42
So I'm looking forward to that.
28:43
I'm looking forward to getting a little bit of rest,
28:45
and then I'll decide, you know, what my next steps will be.
28:48
- Ms. So thank you so much for joining us
28:51
and even more thank you for the 27 months
28:54
of incredible service. Thank you.
28:56
- Thank you so very much. Thank you.
28:59
- That brings us to the end of this episode
29:01
of Degrees of Success.
29:03
Don't forget to like, subscribe, and comment.
29:06
I'm your host, Frida Richards, reminding you
29:09
that your next chapter might be your best one yet.
29:13
See you soon.
Chapters in this video
- Growing up in Arizona
- Public health challenges
- Reconnecting with traditional practices
- Cost and access issues in Alaska
- Integrating holistic health
- Education and wellness centers
- Rural health access and challenges
- Personal inspirations and future goals
About UOPX alumna Roselyn Tso
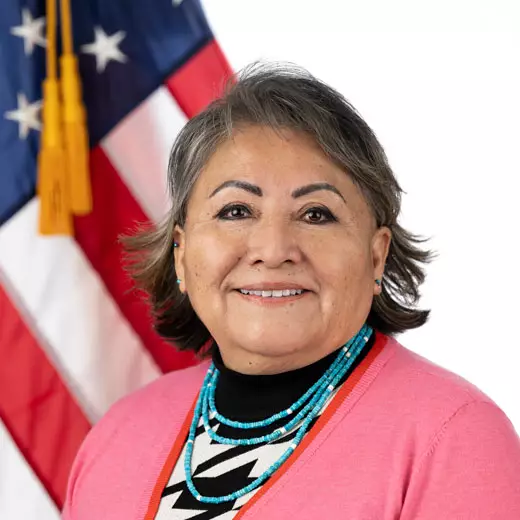
Roselyn Tso is an alumna of Ų▀╔½╩ėŲĄ with a masterŌĆÖs degree in organizational management. As an enrolled member of the Navajo Nation, she served as the 11th director of the Indian Health Service until she . IHS is the 17th largest healthcare system in the U.S. and serves American Indians and Alaska Natives.

About the Degrees of SuccessŌäó Podcast
The Degrees of Success podcast by Ų▀╔½╩ėŲĄ brings you inspiring stories of UOPX alumni who have transformed their careers through education. Each episode highlights personal journeys of overcoming obstacles, achieving professional milestones and using education to unlock new opportunities. Whether youŌĆÖre looking for motivation, career advice or guidance on how education can propel you forward, these alumni stories offer invaluable insights to help you succeed.
